Thermablate is a minimally invasive one time treatment option for pre menopausal women suffering from heavy menstrual bleeding due to begin causes who have completed childbearing

 The Thermablate Endometrial Ablation System is a clinically proven, gentle, two minute treatment that can significantly reduce or stop heavy menstrual periods for women who have completed childbearing.
The Thermablate Endometrial Ablation System is a clinically proven, gentle, two minute treatment that can significantly reduce or stop heavy menstrual periods for women who have completed childbearing.Thermablate EAS is a one-time, non-hormonal treatment that reduces the need for major surgical intervention such as hysterectomy.
How does it work?
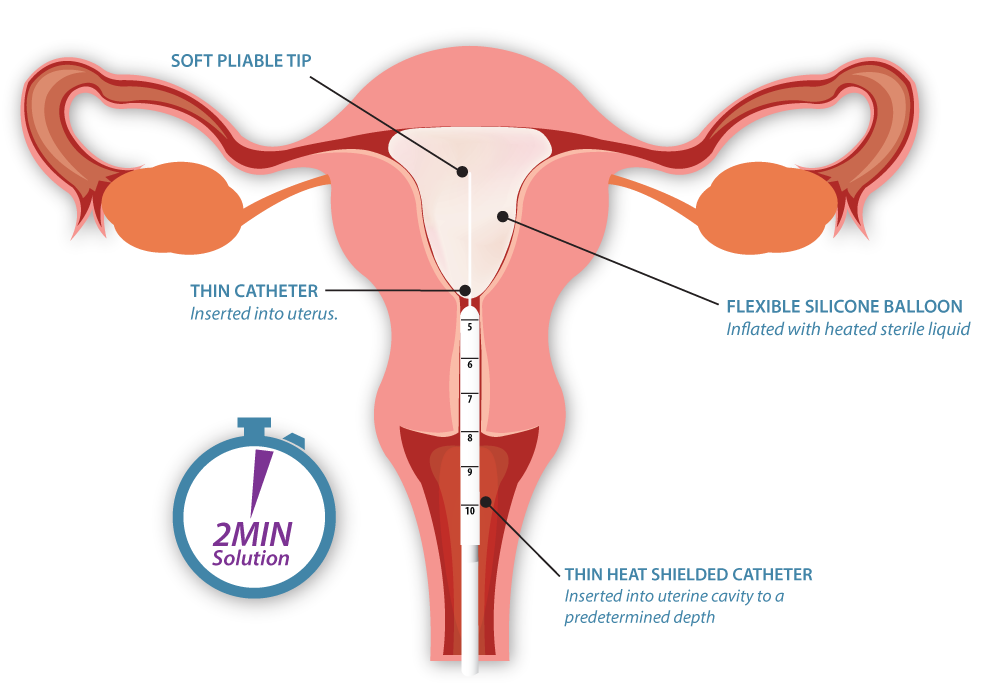
The Thermablate EAS is made up of a Treatment Control Unit (TCU) and disposable cartridge, often referred to as a balloon catheter.
A TCU is:
- Fully automated
- Simple to set up
- Compact, lightweight
Proper patient selection is very important to consider. Not all women can undergo a Thermablate treatment. Patients should always be evaluated thoroughly prior to treatment to rule out any underlying causes of their excessive uterine bleeding.
Potential Thermablate patients must meet certain criteria to be eligible for treatment:
- Excessive uterine bleeding with no underlying causes
- Completed childbearing
- Pre-menopausal normal uterine cavity with sounding between 8cm and 12cm, inclusive
- Normal endometrial biopsy and pap smear in accordance with Clinical Practice Guidelines
Contraindications
It is important to rule out contraindications prior to treating a patient with the Thermablate system. Most importantly, patients should understand that becoming pregnant after a Thermablate procedure is possible but it may be unsafe for both the mother and the fetus. Proper birth control counselling should be provided to patient’s pre and post procedure.
Repeat endometrial ablations should not be offered or attempted with Thermablate EAS as the uterine cavity is likely distorted.
- User slowly inserts catheter until balloon tip touches the fundus of the uterine cavity
- Depth markings on catheter must match previously obtained sounding measurements
- Treatment cycle is activated with a simple finger trigger switch
- Thermablate system automatically inflates and deflates the balloon to ensure consistent delivery ofenergy and contact with the endometrium
At Two Years
- Up to 98% of patients reported return to normal menstrual bleeding, hypomenorrhea or amenorrhea1
- 82% of women were satisfied with their treatment2
At a Median of Five Years
- 93.6% of women avoided hysterectomy3
- 80% of patients experienced reduction in menstrual bleeding and required no additional therapy. 6.4% underwent hysterectomy3
Success Measured as Improved Quality of Life
Thermal balloon ablation offers many benefits over competitive Global Endometrial Ablation systems and is the ideal treatment option for avoiding long-term complications such as De Novo (newly onset) Pelvic Pain.
“De Novo pelvic pain occurred overall in 20% of radiofrequency patients and 7% of Thermal Balloon patients” 4
A study comparing the incidence of De Novo Pelvic Pain within 2 years of either Radiofrequency (RF) or Balloon Ablation found that:
- More focus is being placed on improved quality of life rather than solely menstrual patterns post ablation
- The possibility of De Novo Pelvic Pain post-ablation should be reviewed with the patient pre-procedure
- The incidence as well as its associated severity varies by mode of therapy (RF>TB)
A retrospective review comparing outcomes of patients treated with Thermablate (N=175) and Novasure (N=133) over 5 years showed “An eventual hysterectomy was carried out in 18.7% of the Novasure women vs 8% of the Thermablate group.” 5
These data are further supported by the findings in Figure 2, which shows that of 3861 endometrial ablations performed from 1999-2004, a larger percentage of patients treated with Radiofrequency (NovaSure) ablation underwent eventual hysterectomy when compared to Thermal Balloon patients. 6
CONTACT US TODAY